




Findings
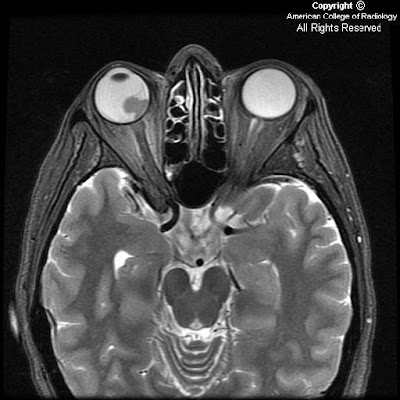
Thin section axial fat-suppressed fast spin-echo T2-weighted imaging
Figure 1 and Figure 2 show a V-shaped retinal detachment pointing toward the optic nerve. There is increased T1 signal posterior to the detachment suggesting hemorrhage.
Thin section axial fat-suppressed T1-weighted imaging
Figure 3 and Figure 4 show a mass arising from the nasal aspect of the right ocular globe. There is a collar button configuration to this mass, which assumes the typical configuration strongly suggesting elevation of Bruch’s membrane. The mass is near isointense to muscle on precontrast T1 and T2 weighted images. This mass extends towards the vitreous but no extension beyond the sclera is identified.
Postcontrast fat-suppressed T1-weighted imaging
Figure 5 and Figure 6: The mass is near isointense to muscle on pre-contrast T1 and T2 weighted images and demonstrates prominent contrast enhancement.
Diagnosis: Malignant melanoma of the uvea
Uveal melanoma is the most frequent primary intraocular malignant tumor in adults. It is rare in children. Its importance is that it is the main intraocular disease that can be fatal in adults.
Uveal melanoma can erupt through Bruch's Membrane. When this occurs, they develop a characteristic collar button configuration that extends through the vitreous chamber.
Uveal melanomas have differing MR characteristics, depending on the amount of melanin, which has paramagnetic properties. Melanomas containing a lot of melanin will demonstrate T1 hyperintensity, and markedly decreased T2 signal. However, in amelanotic or slightly melanotic melanomas, the typical MR pattern is isointense on T1, and slightly hypointense on T2.
Uveal melanoma is the most frequent form of intraocular malignancy in adulthood (4). As the uvea is the most vascular region of the globe, it is a common site for primary and metastatic neoplasm. Uveal melanomas comprise 70% of malignant intraocular tumors. It affects approximately 5-7 out of 1,000,000 people (3). Uveal melanoma can occur in any of the three subdivisions of the uvea: the iris, ciliary body, and choroid.
Uveal melanomas start with a flat growth profile along the choroid. With progression, they become elevated, and frequently extend through Bruch's membrane, where they can track into the subretinal space. With spread through Bruch's membrane, the melanoma can have a "mushroom shape" or "collar button" appearance that extends through the vitreous chamber.
Uveal melanomas typically appear as a solid, well-defined mass on magnetic resonance imaging. Melanin is paramagnetic, so in melanomas containing a lot of melanin, there is increased T1 signal with markedly decreased T2 signal. This signal intensity pattern is pathognomonic for uveal melanoma, as there are no other intraocular lesions with this appearance. In low-melanin or amelanotic melanomas, Magnetic Resonance imaging is less specific, but typically shows isointense signal on T1-weight images and slightly hypointense signal on T2-weighted images. Uveal melanomas typically have moderate to strong contrast enhancement following administration of gadolinium.
B-mode ultrasound typically shows a rounded, hypoechoic, highly vascular lesion. Retinal elevation and vitreous hemorrhage can also be seen, as these are complications of uveal melanomas. Uveal melanomas on unenhanced computed tomography appear sharply marginated, hyperattenuating, and elevated.
Uveal melanomas also have a propensity to metastasize hematogenously, and do so most frequently to the liver. Uveal melanoma is the most common fatal intraocular disease in the adult population.
Optimal treatment for uveal melanomas is controversial and clinical trials are ongoing. Large melanomas, typically greater than 10-mm in thickness, are usually managed with enucleation. For medium sized melanomas, 3-mm to 10-mm thick, plaque brachytherapy and external-beam radiation therapy have been accepted as alternatives to enucleation. For small lesions, less than 3-mm, routine monitoring with ultrasound is recommended as these may represent benign choroid nevi. These small lesions may also be biopsied, with a positive result placing the small melanomas into the medium melanoma treatment category.
Prognosis is dependent on many factors. Increasing tumor pigmentation is associated with a less favorable prognosis. Additionally, increasing size, infiltration through Bruch's membrane, and retinal detachment are all associated with a poorer prognosis. In metastatic disease to the liver, the mean survival has been reported to be nine months.
No comments:
Post a Comment